On July 13, 2021, the Centers for Medicare and Medicaid Services (CMS) issued its calendar year 2022 Medicare Physician Fee Schedule (MPFS) proposed rule. This annual rule, which sets Medicare physician payment policies for the following year, if finalized, would implement provisions resulting in devastating undervaluation of certain EP services.
March 2022
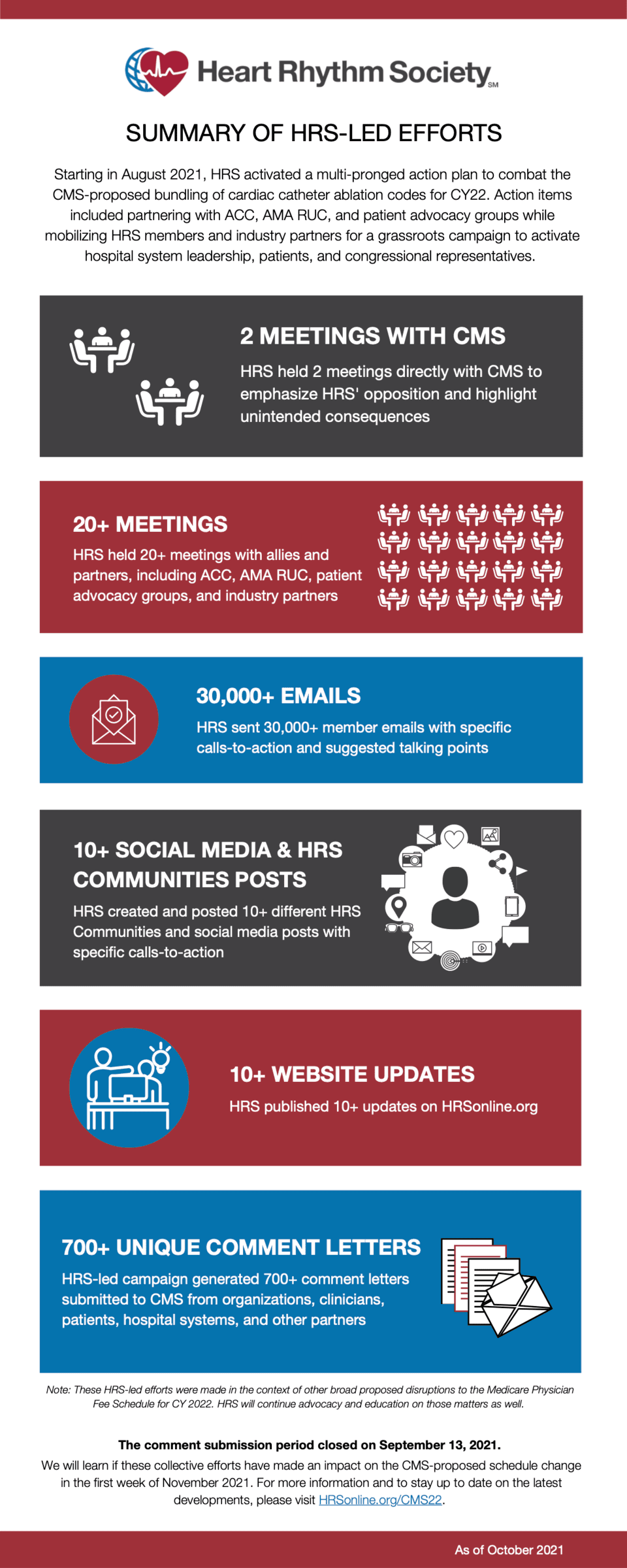
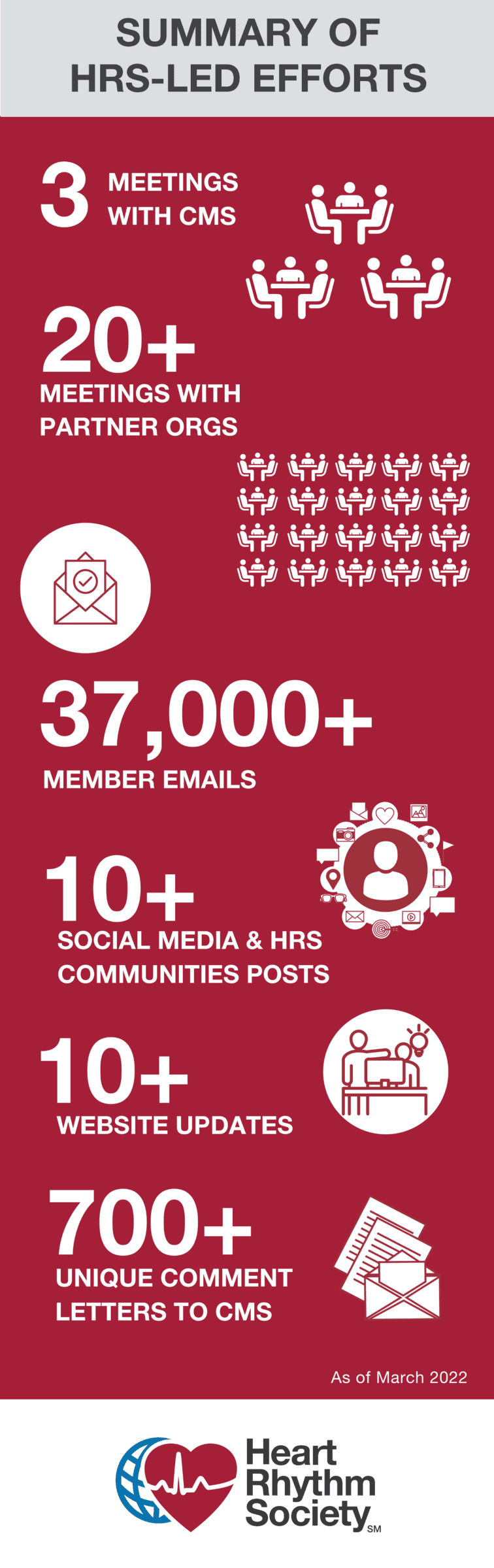
Summary of HRS efforts to prevent reductions to ablation reimbursement by CMS
December 20, 2021
In its final rule in November 2021, the Centers for Medicare and Medicaid Services (CMS) ultimately did not change course. In direct contradiction to requests from HRS, ACC, and the AMA RUC, the final rule maintained the old value of the base codes with no additional compensation for the add-on codes.
November 2, 2021
CMS released the CY 2022 Medicare Physician Fee Schedule (MPFS) and Hospital Outpatient Prospective Payment System (OPPS) Final Rules. The cardiac ablation codes were finalized as proposed.
The final rule puts forward a CY 2022 MPFS Conversion Factor (CF) of $33.5983. This includes a slightly modified CY 2022 budget neutrality adjustment of only 0.10% — it was 0.14% in the proposed rule. However, the overall drop in the CF from CY 2021 is still over 3.7% due to the expiration of the Congressional 2021 payment increase of +3.75%.
While HRS is disappointed with the final rule, learning that CMS will consider the RUC recommendations in 2022 offers hope that there could be a slight increase in 2023. HRS, alongside our members, partners, and patients will remain diligent in the fight for fair compensation and the prevention of unintended consequences.
MPFS
Full Ruling | CMS MPFS Press Release | CMS MPFS Fact Sheet
OPPS
October 27, 2021
The comment submission period closed on September 13, 2021. HRS expects to learn if its joint efforts had an impact on the proposed code changes during the first week of November 2021.
In the meantime, HRS would like to thank all of the HRS members who contributed their time and expertise to combating these proposed changes. Additionally, HRS thanks its allies and partners in this fight, including the American College of Cardiology (ACC), the American Medical Association RVS Update Committee (AMA RUC), patient advocacy groups such as StopAFib.org, and industry partners.
Together, our grassroots campaign to activate hospital system leadership, patients, and congressional representatives ensured that the EP community's collective voice of deep concern was heard.
August 31, 2021
HRS submitted its recommendations to the Centers for Medicare and Medicaid Services (CMS) on the Agency's proposed payment impact to EP services under the Medicare Physician Fee Schedule for Calendar Year 2022.
August 15, 2021
What can you do?
- Write and submit your own letter to CMS before the September 13, 2021, deadline. Please reference these additional resources to help you get started. It is important to note that CMS will likely disregard your letter if it contains recurring boilerplate language. Thus, HRS recommends expressing your thoughts and concerns in your own words.
- Talk with your hospital system to ensure their awareness of these proposed cuts and convince them to submit their own letters to CMS.
- Contact your federal lawmakers to ensure they are aware of the cuts and the impacts these cuts will have on healthcare delivery.
Remember, comment submission deadline is September 13, 2021.
August 14, 2021
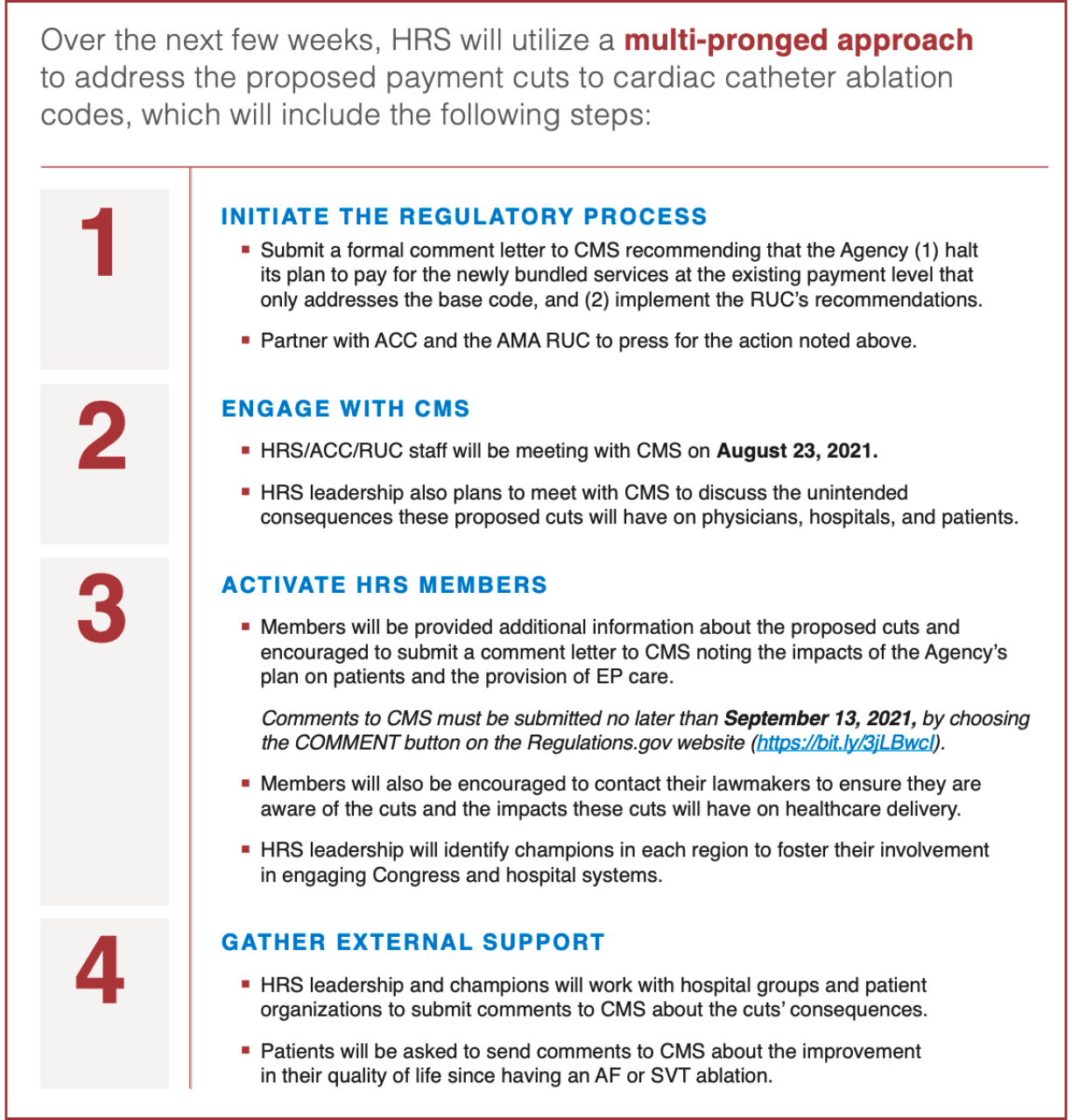
HRS Action Plan to Address Proposed Cuts
This extreme CMS undervaluation of ablation services is of the highest priority and HRS will vigorously advocate on behalf of you, your patients, and the services that you perform.
Since the release of CMS' proposed physician payments for 2022, HRS has been collaborating with the American College of Cardiology (ACC), the American Medical Association's Relative Value Scale Update Committee (RUC), and industry partners to develop and deliver a unified response.
On August 24, 2021, HRS, ACC, and RUC staff will meet with CMS leaders to learn more about the Agency's decision to propose these drastic cuts and to recommend that CMS apply the RUC's recommendations. HRS President Fred M. Kusumoto, MD, FHRS, will also arrange a meeting with CMS and fellow HRS leaders to discuss the unintended consequences that the proposal will have on patient care, EP programs, and hospitals.
HRS will submit a comment letter to CMS before the submission deadline on September 13, 2021. The CY 2022 MPFS final rule is expected in early November 2021.
July 13, 2021
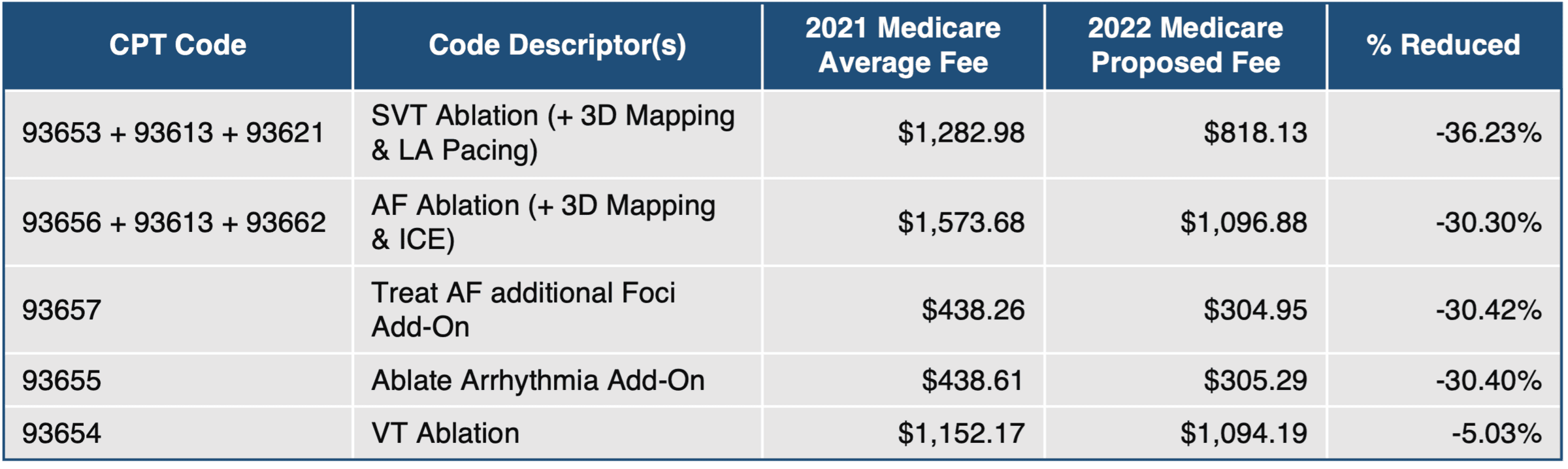
Proposed Changes
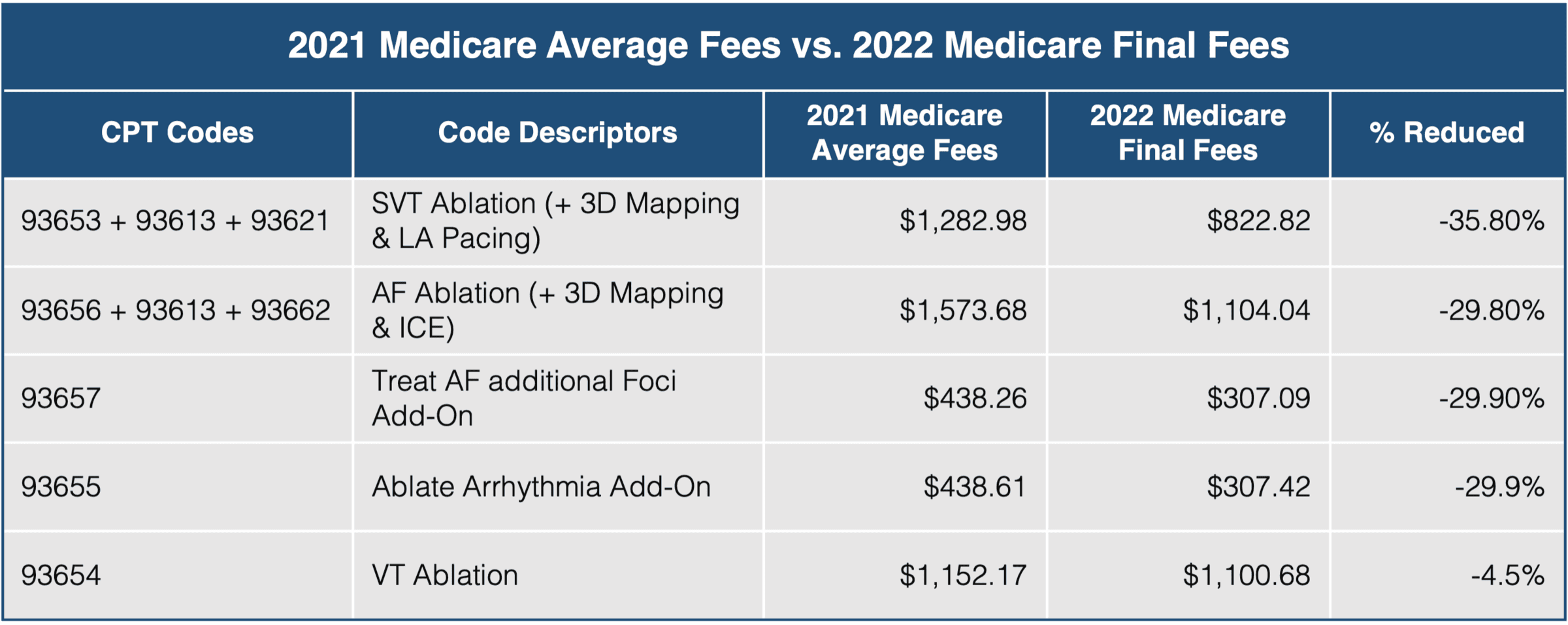
*As of August 17, 2021
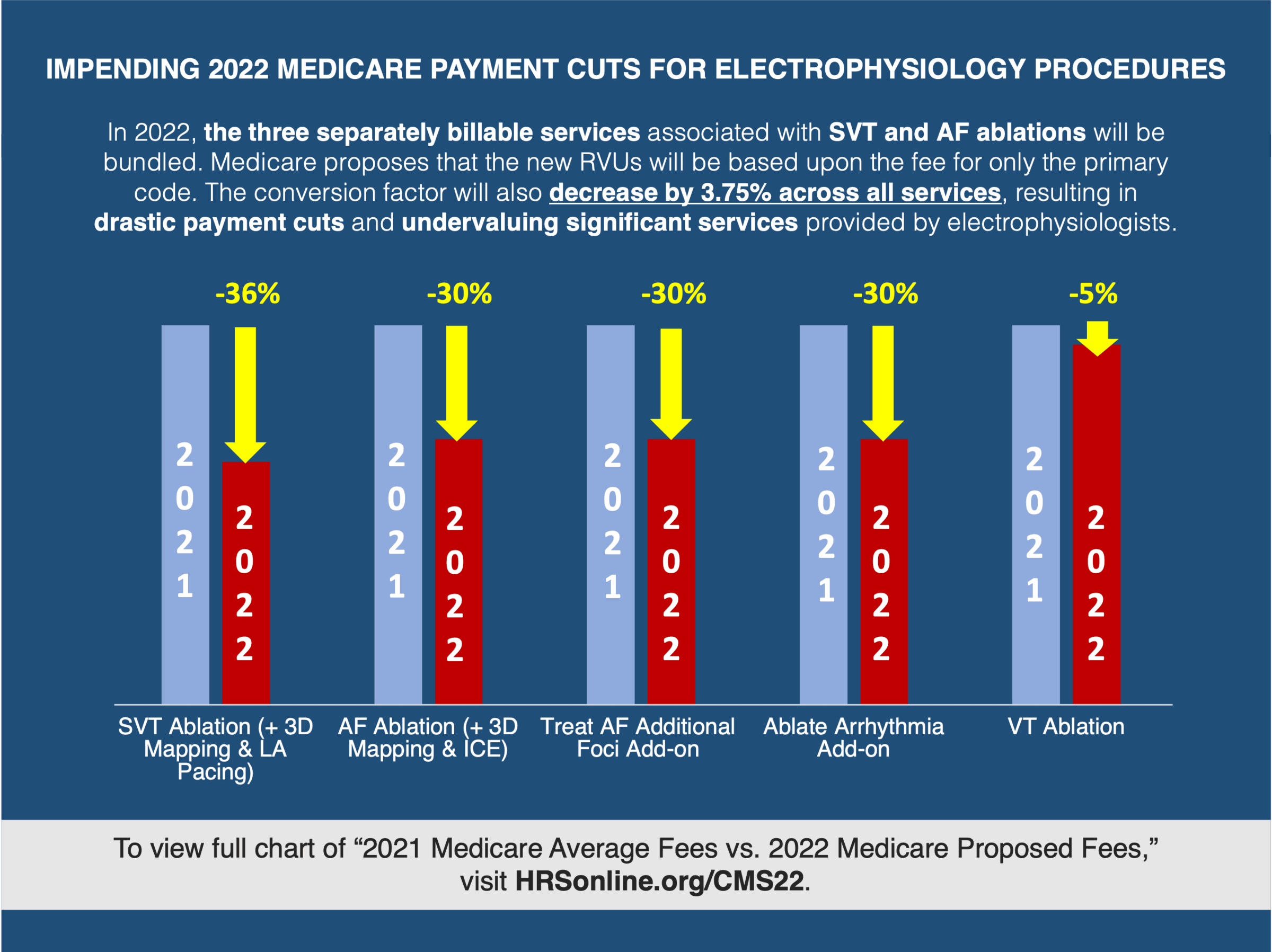
CMS Proposes to Reduce the MPFS Conversion Factor by Nearly 3.75%
If finalized and without Congressional intervention, the CY 2022 MPFS conversion factor would be reduced by nearly 3.75%, going down from $34.8931 in 2021 to $33.5848 in 2022. This reduction would span across all services and continue the sustained assault on overall Medicare payments. HRS will urge CMS and Congress to avoid these continued financial pressures on physician practices while Medicare payments to facilities continue to see year-over-year inflationary increases in their payments. These cuts could be exacerbated by the 2022 sequestration cuts expected if Congress does not intervene.
CMS Proposes to Ignore Recommendations on Work Valuation for Bundled Ablation Services
As expected, CMS addressed the work values for revised CPT codes 93653 (SVT ablation) and 93656 (AF ablation). CPT codes 93653 and 93656, typically furnished in conjunction with add-on codes CPT 93613, and CPT 93621 or 93662, were expected to bundle the services associated with the add-on codes. In conjunction with that bundling, the work RVU value was expected to increase to reflect that the services in the add-on codes were now bundled into the base codes. However, CMS has inexplicably proceeded with the bundling of the add-on codes into the base codes without any congruent increase in the work values of the base codes to reflect the increased level of service. HRS vehemently opposes the CMS decision to maintain the work values for a base code that is now intended to reflect the work associated with previously billed add-on codes. This undervaluation of EP services is unjustifiable, and HRS will work with CMS, ACC, and the AMA to prevent these unsubstantiated cuts to services that you provide and from which patients benefit every day.
CMS Proposes Drastic Fluctuations in Practice Expense RVUs
HRS will continue to analyze the proposals and provide additional information. However, the proposed rule will also have a significant impact on reimbursements for practice expenses (PEs). For example, due to a combination of the new bundling policy and other PE changes made in the rule, RVUs for PE for CPT 93653 will drop by approximately 35% under the new proposals[b3] if CMS continues to treat the add-on codes as bundled even though it inappropriately refused to make requisite changes to the RVUs.